I have always respected your posts so when I saw your title was about iron deficiencies I was buckled in. You know that old adage, "when the newspaper reports on your area of expertise it's crap, and yet you believe the rest of it" - I always pay special attention to what people I trust/respect say about things I know a lot about, especially when there's a lot of misinformation out there.
I have just completed the requirements for a bachelor's degree in Nutrition with a focus in biochemistry. I am not a dietitian and will freely admit I know less about iron than you do after this lit review. But what you said makes sense and is scientifically grounded and dovetails with the stuff I know "formally". tl;dr I am thrilled to know that I can trust all your future posts.
I did recently write a draft blog post about iron aimed at a general audience as part of an internship, and I think a few of the things I say in there will provide useful context and background.
And yes, menstruating is definitely the reason why women are recommended more - I found the original paper where that recommendation comes from and that's what they talk about.
One thing I have to add - 'black stools' are also a common side effect of iron supplementation, as well as constipation, that doesn't mean you have iron toxicity. But taking "chelated iron" avoids that side effect.
Before I start talking about iron, I want to take a step back and talk about two concepts in nutrition that are often not well communicated to the public: the RDI and the EAR.
You’ve probably seen food labels that talk about the “% RDI” of different nutrients, and you might even know that it stands for “recommended dietary intake”. There’s another concept that goes along with it that you won’t find on nutrition labels: the EAR, or “estimated average requirement”. The RDI is the daily intake that will be enough for 97.5% of people, and is used when checking if an individual is consuming enough of a nutrient. The EAR is the intake that will be enough for 50% of people, and is used in nutrition research to check if a population is consuming enough of a nutrient.
These numbers are pretty close for most nutrients, but for iron they can be very different. The iron RDI for adult men is 8 mg/day and the EAR is 6 mg/day. Similarly, the RDI for post-menopausal women is 8 mg/day and the EAR is 5 mg/day. So the RDI and EAR are 2-3 mg apart. In comparison, for women who menstruate, the RDI is 18 mg/day and the EAR is 8 mg/day — a 10 mg difference!
To put that in concrete terms, imagine 100 women of childbearing age in a room (and none are pregnant or breastfeeding). 50 of them would be perfectly healthy consuming 8 mg or less of iron a day. 48 would need between 8 mg and 18 mg a day. And two of them would need even more than 18 mg!
So, even though the food labels recommend 18 mg of iron for women in this age range, half of them will have enough iron eating less than half the recommended amount — and 2% will need even more than the recommendation! This is why some people will have low iron levels, and other people who eat almost identical diets will have good levels. There’s a lot of variation in iron needs in this particular group and it comes down to variability in menstrual losses: for example, some women in this age group don’t menstruate at all and some may experience very heavy periods.
I’ve noticed this in the vegetarian community: a lot of people will say vegetarians don’t need to take iron supplements because their own iron levels are great, citing spinach or some other iron-rich vegetable as the reason for this. A cup of raw spinach contains 0.8 mg of iron, and the RDI is 18 mg. A typical daily “women’s multivitamin” contains around 5 mg of iron, the equivalent of 6 cups of raw spinach, every single day! For comparison, 100g of tofu contains about 3 mg of iron and 100g of beef contains about 3.5 mg of iron. It is most likely that people claiming that they don’t need iron supplements happen to be ‘lucky’ and need lower intakes.
On the subject of vegetarianism, contrary to popular belief, vegetarians and vegans tend to consume about the same amount of iron as people eating a typical western diet and are at similar risk of deficiency (https://academic.oup.com/ajcn/article/70/3/353/4714844 and https://www.mja.com.au/journal/2013/199/4/iron-and-vegetarian-diets ). However, due to the reduced absorption of iron from plant foods (18% is absorbed from a mixed western diet but only 10% from a vegetarian diet), it is recommended that vegetarians consume 80% more iron.
This is because there are two types of iron: heme iron, from animal sources, and non-heme iron, from plant sources. Heme iron is more easily absorbed, which is why vegetarians need more iron. A misconception about heme and non-heme iron is that all iron in meat is heme, but in fact, more than half of iron in meat is non-heme. So, 100g of beef would contain about 2 mg of non-heme iron and 1.5 mg of heme iron, while 100g of tofu contains 3 mg of non-heme iron. Non-heme iron absorption can be improved by consumption of vitamin C, which is abundant in most vegetarian and vegan diets.
So, where does all that leave us?
The only way to be sure of your iron status is to have a blood test, as I recommended in the previous article [unpublished; basically a much simpler version of the OP]. If your levels are low, you may want to incorporate more iron-rich foods in your diet, and ensure you consume vitamin C around the same time. You may also want to consider a supplement, especially if you have heavy periods. Whatever you do, you should get follow-up blood tests to ensure that it is working.
Iron supplements can often cause dark stools and constipation, so you may want to try several brands to find one that works for you. Some iron supplements contain “chelated iron”, which is more gentle on the stomach. [plug for advertised product removed]. For treatment of deficiencies under appropriate medical supervision, high-dose Ferrograd-C is available from pharmacies [in Australia]—though this contains non-chelated iron.
Finally, do not take high doses of iron supplements outside of medical supervision: they can be dangerous.
What's your opinion on reference ranges? My understanding is that they're often too wide, that the minimum is what you need to avoid deficiency diseases but won't get the average person to optimal function (although there exist outliers for whom it's exactly the right amount). So the RDI is set too high for most people but the reference range too low for most people. But I've never dug into this besides my research on iron not turning up anything on optimal functioning, just deficiencies. Which is maybe fine because knowing the average optimal amount isn't that informative about your personal optimal amount, that requires self experimentation?
IIRC, RDIs (and I would guess EARs) vary quite significantly among the various organizations that calculate/estimate/publish them. That might be related to the point ChristianKI seemed to be trying to make. (Tho I don't know whether 'iron' is one of the nutrients for which this is, or was, the case.)
I'm not sure whether or not to take this post as evidence that the field of nutrition is diseased or not.
The RDI is not what is enough for X amount of people but what is thought to be enough by a given authoritative body that published the RDI. While I do hope that there's some correlation between what's recommended and what's actually needed, people in the field confusing their abstractions and ignoring a portion of their uncertainty is a bad sign.
Sorry I only just saw this post. I would not classify myself as "in the field", for what it's worth. I would consider "my field" to be traffic engineering, as I have 10+ years experience in that (not including undergrad). My experience in the field of nutrition is less than that (a 3 year undergrad degree).
The main part of my post is a blog post I made aimed at an intelligent lay audience, so I did leave some nuances out. I do not consider the fact that the NRVs are published by a body that doesn't (and with current technology can't) know the "true" RDI to be the major shortfall that you clearly think it is.
Personal anecdote so obviously all n=1 caveats apply - I took light iron supplementation for a few months (one Spatone sachet per day) and it completely changed my life. Before, I could not run more than a mile, in 10 minutes, before collapsing. I got winded going up stairs, was often physically fatigued (although no other mental or non-fitness-related physical symptoms). After a few months of iron and no other lifestyle changes, I could run for an hour at 8 min/mile pace. Have stopped taking the supplements and benefits have sustained for 2 years. If you have mild iron deficiency, I really do suggest addressing it as the lifestyle gains could be really big, and I can recommend Spatone iron water as a delivery mechanism with fewer side effects.
If the the benefits persisted for two years after ceasing to take the iron, doesn't that suggest that iron wasn't actually the causal factor? Or am I missing something here?
It's possible that once my iron reserves were replenished through supplementation, the amount of iron needed to maintain adequate levels was lower, allowing me to maintain my iron status through diet alone. Iron is stored in the body in various forms, primarily in ferritin, and when levels are low, the body draws upon these reserves.
I'll never know for sure, but the initial depletion of my iron reserves could have been due to a chest infection I had around that time (as infections can lead to decreased iron absorption and increased iron loss) or a period of unusually poor diet.
Once my iron reserves were replenished, my regular diet seemed to be sufficient to prevent a recurrence of iron deficiency, as the daily iron requirement for maintenance is lower than the amount needed to correct a deficiency.
If you're vegan and drink lots of tea (guilty), consider avoiding tea at least one hour before and after the time you eat iron-rich food. The worry is that polyphenols in tea bind with non-heme iron, forming a stable-ish complex that prevents absorption. There's weak evidence that this makes a practical difference, but it was especially relevant for me since I drink tea almost exclusively.
From the available evidence there is no need to advise any restriction on tea drinking in healthy people with no risk of iron deficiency. In groups at risk of iron deficiency the advice should be to drink tea between meals and to wait at least 1 h after eating before drinking tea. (source)
Most studies have found no association between tea intake and iron absorption. However, drinking excessive amounts of black tea may inhibit the absorption of iron, and may harm people with anaemia. (wikipedia)
From Preston Estep's Mindspan:
As a result, men in Crete have a biological age about five years younger. They also have ferritin levels about half the average level in Zutphen, which is consistent with their significantly lower risk of stroke, cancer, diabetes, and heart attack.
According to Japan’s 2006 National Health and Nutrition Survey, people in Japan and Okinawa also have low ferritin, and a large proportion are iron deficient (50 percent of women of childbearing age have ferritin below 20 ng/mL). Japanese also have low hemoglobin.
The World Health Organization defines anemia as hemoglobin levels below 12 g/dL for women and 13 g/dL for men. This difference in minimum acceptable value for men and women is arbitrary, simply because women tend to have lower levels—not because a value between 12 and 13 g/dL is unhealthy for men. The average hemoglobin levels for older Japanese (including centenarians) are often even lower than this minimum. In a publication from 1996, average hemoglobin levels in healthy Japanese centenarians were reported to be 11.5 g/dL for women and 11.8 g/dL for men. We can’t be certain that their hemoglobin has always been so low, but we can be sure that their diets and lifestyles haven’t changed much, and these values are lower than those measured in elderly people in Mindspan Risk countries.
Estep recommends ferritin of 10 to 40 ng/ml (mine is 89)...
Animal studies show that high iron feeding increases body iron stores and shortens lifespan, and adding tea to the diet reduces body iron and increases lifespan. In late 2015, a study of people who ate a Mediterranean-style diet (characterized mainly by less meat and more fish) had larger brains and key brain structures and less atrophy than frequent meat eaters. The difference between the two groups that ate the most and least meat was equivalent to five years of brain aging. And of course there are the Mindspan Elite and their lower body iron stores and lower rates of Alzheimer’s. Taken together, this evidence is very strong, but these studies don’t show direct cause, as a clinical trial does. That’s been done too. In 1991 the iron chelator drug deferoxamine* (which binds iron and renders it inactive) was shown to slow the progression of Alzheimer’s disease.
I am not a doctor, my most relevant credential is a BA in a different part of biology, the fact that I couldn’t find a decent resource and had to make it myself is a sign of civilizational inadequacy.
I am not sure what your definition of a decent resource is, but I googled "iron deficiency non anemic" and read the first result, Iron deficiency without anaemia: a diagnosis that matters (by a group of medical students and a haematology consultant, from 2021). It contains:
- An explanation of how IDA (iron deficiency anaemia) and IDWA (iron deficiency without anaemia) differ, and how IDWA is an overlooked and important issue.
- A more detailed and nicely diagrammed algorithm for diagnosing ID (IDA or IDWA) that also addresses people with chronic inflammation, who need a different testing approach
- A nice, detailed explanation of the causes of iron deficiency and iron's many roles in the body beyond haemoglobin and myoglobin synthesis. It contains jargon, but is about as accessible as a standard textbook, and I found it more readable than the average scientific paper.
- A more comprehensive list of types of people who might suffer iron deficiency (also including growing children, pregnant women, athletes, those with chronic inflammation, bariatric surgery patients, those with autoimmune gastritis, consumption of coffee, tea or calcium, blood loss as in menorrhagia, etc).
- Detailed explanation on how to manage iron deficiency, including a nicely diagrammed algorithm
What this source lacks that your post contains is a detailed and critical breakdown of specific studies. It contains more jargon and might be more detailed than a layperson would want to read. It also lacks a component of directly encouraging people to proactively get tested for iron deficiency, being addressed mainly at doctors rather than at patients. While I think it's readable and motivating for a scientiifc paper, it's not as galvanizing or readable as your blog post.
As you go about writing more research articles, I think it would be really helpful to be specific about what it is that you are missing in the resources you come across. I have shown a couple of your recent pieces to a medical student friend of mine, who's particularly interested in exercise and nutrition and has also suffered severely from a missed diagnosis. He finds your writing interesting, but also somewhat offensive, oversimplified, and potentially steering patients toward ineffective self-testing that may actually cause false negatives and lead people to think they've tested themselves for iron deficiency and it's not a problem, when they are in fact iron deficient.
Not being a doctor, I don't really get offended by your writing, but I've been interested in the question of oversimplification or misdirection of patients. That is why I chose to look up this article and see what it has to offer. I am curious to know more about whether you came across it, and what if anything you think it lacks that your blog post addresses.
This could be read as a critical and contentious response to your piece, but I hope you will receive it in the spirit that it's meant - me attempting to better understand your motivations as a writer and the larger objective of the medical research you are doing. Thanks.
This seems like a pretty good article for its goals (plus it immediately confirms my claim that existing infrastructure handles IDWA poorly "IDWA is poorly recognised by clinicians despite its high prevalence, probably because of suboptimal screening recommendations", which is nice). I think it is borderline useless for my goal of getting readers, especially ethical vegans, to go from not caring about iron deficiency to taking action.
I did a fair amount of ~market research with the target audience; people are very lazy and there is a lot of competition for their attention. I spent an immense amount of time generating hard numbers and figuring out how to present them in a way as accessible and motivating as possible without misleading people or catching the wrong audience. This is extremely hard, and AFAICT the Al-Naseem paper isn't even trying, because it is aimed at a different goal.
I only skimmed the article, and maybe I missed the part where it quantified the costs of IDWA or provided an algorithm for treatment (as opposed to diagnoses, which I do see). But since the entire point of this post was surviving skimming, I consider that a fair criticism of it for the purpose of motivating lay-readers.
It sounds like you and your doctor friend are treating the counterfactual to this post as "competent, thorough medical care". I think this is incorrect; the counterfactual is nothing. I informally polled Lightcone vegans, and there was a variety of interactions with the medical system and nutrition, including "absolutely nothing", "testing recommended but not done", and "got tested but was missing tests that obviously should have been done". This includes people who had obvious symptoms that could plausibly be caused by their vegan diet. Obviously, some people had seen doctors and gotten proper treatment, which is great and I wish happened more often. But this post is aimed at the people who hadn't and weren't going to.
If the effort I spent writing this post could instead have gotten everyone reading it competent medical care, I would have done that.* And I will say for the record that no one should treat this as a substitute for medical treatment. But as an alternative to nothing, I think it holds up quite well.
*In fact I toyed with "find excellent doctors in the bay area" as a project, and decided against it because it would have been pretty costly for me, and I didn't find enough people I expected to act on the information even if I succeeded. I think it's plausible people underestimated their own demand once someone really great was found, but the most likely funder was FTXFF so I'm pretty happy I didn't go through with it.
Thank you for this thorough response. Let me clarify that my med school friend and I have distinct angles on this post, neither of which, I think, is 'the counterfactual to this post is competent, thorough medical care.' We are both quite aware of the shortcomings of the medical system and we both know that patients aren't always as proactive as they should be in treating real medical problems.
I won't speak for him, but I mentioned in my comment above that your paper stands out from the al Naseem paper I linked in being more "galvanizing and readable," as well as in breaking down specific studies. This helps me understand that your central objective is to motivate readers, especially ethical vegans, to get adequately tested for iron deficiency, and that you've crafted this article to appeal to your specific readership. That wasn't entirely clear to me when I read your post, and I understand better where your posts are coming from now that I understand the legwork you're doing behind the scenes. Thanks for sharing.
Can I ask, a year later, why you didn't reply to the person who cited evidence that low iron is good?
Of the comments, that one seems by far the most productive for you to engage with, at least for me as an almost-zero-knowledge reader (and recently converted ethical vegan who is eager to mitigate any health tradeoff). But it's the only upvoted comment you haven't replied to! I'd be really interested in what you have to say about it.
I don't know which comment you're referring to, since the grandparent of yours isn't about excess iron.
I can say (as I did many times in the post) that in general I believe excess iron is bad. I also believe that excess starts earlier than what the medical system recognizes as a problem, symmetrically to having too low a threshold for iron deficiency. I haven't dug into where the threshold for excess lies, and suspect it varies a lot by individual. If someone gave more specifics on the line for excess I'm grateful, but probably wouldn't have much to add because I've only looked at the low end.
It's almost the only comment you haven't replied to, aside from the downvoted ones at the bottom. Third one down if your comments are sorted by top scoring, which I assume is default? It's by Alex K. Chen.
It honestly seems kind of hard to miss, and cites some interesting suggestive evidence that low iron levels could actually be healthy, which is why I asked.
Did you know you can link directly to comments on LW? It's the timestamp/chainlink icon by the author's name.
The provided evidence looked weak to me, and based on other conversations I've seen with Alex Chen I didn't expect digging into it to be productive. If you're concerned I encourage you to investigate the research yourself or just run some n=1 experiments.
I didn't, thanks! I'm a fairly long-time visitor but sporadic-at-best commenter here, primarily because I feel I can learn much more than I can contribute (present case included).
I'd love to know why you think it's weak. As I mentioned before, it doesn't seem any more than suggestive to me (and to be fair Chen acknowledges as much), but it does seem quite suggestive, and it has introduced a hint of doubt in me.
I get the sense that I've gotten your back up slightly here, which is perhaps not without justification as I admit to having been a touch suspicious of your ignoring the comment and then coming across as a touch uncooperative when I pointed it out. Especially in the context of having noticed, long before converting to veganism myself, that your posts and engagement in subsequent comments struck me as being, in emphasis, framing and tone, somewhat adversarial to veganism.
But I'm well aware that I am probably excessively sensitive to that, having been astonished at the irrationality and extremity of the opposition to veganism online since I converted and before. I'm not sure there's a single moral/political issue where the epistemic and discursive standards are so low (not confined to the omnivores by any means, although it doesn't seem symmetrical to me either). On reflection that has probably clouded my impression (and I notice that I was completely wrong to claim Chen's was the only upvoted comment you ignored, a claim I've struck above). So I want to explicitly withdraw any implied criticism, and simply reiterate my interest in your assessment, as someone with relevant knowledge of and engagement with these nutritional questions. You have previously (thanks again for the tip!) defended the value of expending significant resources on potentially preventing iron deficiency in some proportion of six vegans; for much less than a sixth of that same cost you could at least get one to be much more motivated to address potential iron deficiency. I'd be very grateful, although I'm sure you have other demands on your time.
To answer your object level question:
- I could generate evidence at least this good for every claim in human health, including mutually contradictory ones.
- The book title "mindspan" pattern matches to "shitty science book"
- the paragraphs quoted pattern match to jumping around between facts, without giving straightforward numbers you can hold in your own mind. Why give percentage of childbearing women below a threshold, but averages for the ultraold?
- "adding tea to the diet reduces body iron and increases lifespan" really? this is what he thinks of as evidence?
- "a study of people who ate a Mediterranean-style diet (characterized mainly by less meat and more fish) had larger brains and key brain structures and less atrophy than frequent meat eaters." lots of potential reasons for this, many of which are areas of deep research
- Data on the ultraold is useless because there's a good chance most of them are lying about their age.
- He didn't cite the most relevant information I know of, that regular blood donation improves health in men. Which probably means Alex wasn't done any investigation into this, he just read a few claims some time.
Thank you, I appreciate that.
I'm about to give a lot of context. This is definitely a little unfair, and subjecting you to anger you are not responsible for. But I do feel like you've opened a can of worms, and it would be meaningful to me for you to put yourself in my shoes, which unfortunately requires a lot of context.
The context:
- The mod team[1] and many authors believe that no one is owed a response,. Some people disagree (mostly people who comment much more than they post, but not exclusively). I think the latter is a minority, although it's hard to tell without a proper poll and I don't know how to weight answers.
- Beyond that: because I write about medical stuff means I get a lot of demands for answers I don't have and don't owe people. On one hand, this is kind of inevitable so I don't get mad at people for the first request. On the other hand, people sometimes get really aggressive about getting a definitive answer from me, which I neither owe them nor have the ability to give. One of the biggest predictors of this is how specific the question is. Someone coming in with a lot of gears in their model is usually fun to talk to. I'll learn things, and I can trust that they're treating me as one source of information among many, rather than trying to outsource their judgement. The vaguer a question the more likely it is being asked by someone who is desperate but not doing their own work on the subject, and answering is likely to be costly with benefit to anyone.
Your question patternmatched to the second type. - As you note, I not only had left many comments unresponded-to, but specifically the comments above and below the comment you were referring to (but made me do the work to find). As far as I'm concerned, telling you I couldn't find the comment and giving an overall opinion was going above and beyond.
- Which I do because sometimes on LW it pays off, and it looks like it did here, which is heartwarming.
- You say that you find omnivores to be worse at epistemics and discourse. My experience is strongly the opposite. These aren't incompatible- the loudest people on every side of every issue are usually the dumbest. But keep in mind that the critics of my work on vegan advocacy are drawn from that crowd.
- You came in suspicious of me on a post where I gave vegans and vegetarians useful tests, with grant money I acquired for this purpose, and helped them find vegan supplements. One of my big frustrations with my vegan critics is that they're treating me like a meat industry shill, when my major actions have been to help vegans stay healthily vegan. I don't think means anyone has to agree with me, but I've barely been able to get critics to acknowledge this and explain why it doesn't change anything for them.
- one person did give a satisfying answer to this. It was educational and I appreciate his response a lot, although it did not ultimately change my mind. You can see our dialogue here.
- I've gotten 10-30 emails and comments from vegans telling me I drove them to get tested and if merited go on supplements, and one comment from one vegan saying I was one factor among many in them restarting small amounts of fish. And in the course of getting his statistics help on this post, I talked my dad into a more ameliatarian diet. So from my perspective I have done considerably more for animals than many vegan advocates.
- You might think that people who start eating meat are less likely to tell me, but like you said, I'm detectably not likely to yell at them for it.
- I think your implication is that I don't care about animal suffering or don't like vegans, and this drives me to attack them through any convenient vector. Neither is true. I care about nutrition because I care about nutrition and have for many years, as my blog will attest to. I also care about epistemics and truthseeking in full generality (and my blog will provide a paper trail for that as well). So from my perspective the story that is some people caused a lot of harm (to animals, human health, and truthseeking within EA) by being not only incorrect, but loudly using dishonest tricks to get their way, on an issue I already cared about.
- AFAIK none of my vegan critics have acknowledged either of those points, which is also quite frustrating.
- You might ask "doesn't this imply you [Elizabeth] should be extra charitable to vegans?". The answer is: I am. That's one reason I'm willing to engage with bad commenters (for one round). I'm also careful to distinguish between vegans and vegan advocates when I complain. If anyone else was this epistemically and materially harmful, in EA or LW, on an issue I cared about, I'd be much harsher.
- You came in suspicious of me on a post where I gave vegans and vegetarians useful tests, with grant money I acquired for this purpose, and helped them find vegan supplements. One of my big frustrations with my vegan critics is that they're treating me like a meat industry shill, when my major actions have been to help vegans stay healthily vegan. I don't think means anyone has to agree with me, but I've barely been able to get critics to acknowledge this and explain why it doesn't change anything for them.
- I find leaving a reply about comment A on comment B, which has nothing to do with comment A, to be bizarre at best and hostile at worst. Even if you didn't know how to link to comments, just giving me the author's name would have cut down on the effort demanded from me.
- Telling Alex "naw man, that's not meaningful evidence" seems like it will lead to less high quality disagreement with my posts, not more.
- A detailed refutation is a lot of work.
- I saw your question to Nina questioning her self-report before I saw this comment. It is in some sense a reasonable question, but in practice I get low quality versions of it all the time and it tends to come from incurious people. Additionally, I didn't like that you were speaking as an authority on her life, when she'd given the appropriate caveats.
So the story from my perspective is: I put in a lot of work to help vegans stay healthy and to protect the epistemic commons of two communities explicitly dedicated to strong epistemics. I bent over backwards to acknowledge animal suffering while doing so. A subset of vegan advocates have responded to this work with with overt hostility and shitty epistemics, generating additional work for me that is of no benefit to anyone. I don't know if those comments make up a majority of comments of all comments or comments from vegans, but they are definitely a supermajority of my emotional memories from those comments.
Now someone comes in demanding answers, without making the barest effort to reduce the work that answering requires. He makes a sinister claim that I'm ignoring criticism, citing evidence that takes seconds to disprove. I know I can't give an answer with level of confidence he seems to want, and it doesn't sound like he's done any homework of his own. This[2] has historically created a lot of work for me with no benefit to anyone.
LW occasionally produces miracles, so I answer, in a way that leaves open the door to a productive exchange. But don't put a ton of work into being nicer to the commenter than he was to me, because that's an unreasonable burden and I have a lot of data that says no amount of work will help.
And then it turned out to be one of those LW stories where someone generally reconsiders their views and apologizes for past behavior, which is great. But I don't regret my decision on a policy level.
I think much of this is quite unreasonable (and some very unreasonable- you "don't like that I spoke as spoke as an authority on her life" because I wondered if what she observed was truly attributable to a causal effect?!), but I don't see the value in going over it, especially as others have made the points I would make about your tone and framing elsewhere. I continue to find your contributions on this topic a little more combative and "soldier mindset" than is ideal, but clearly you strongly disagree. (Although it's tempting to suggest that your admittedly "angry" and "unfair" reply, several times longer than your eventual response to the object level question, is evidence for the prosecution, not to mention that it somewhat calls into question your primary 'it's too much work' defence for ignoring substantive criticisms such as Chen's in the first place.) I don't see the point in continuing to argue about whose team is more rational, in any case; all I wanted was your response to Chen's objections to help inform my new dietary choices (something which, again, you concluded was worth dozens of hours and tens of thousands of dollars when multiplied by six, a matter of months ago).
With all that in mind, I have a few follow-up questions to your object-level response, but I will understand if you choose to ignore them, given that you don't seem to enjoy or value the interaction and I'm finding it lower value than I'd hoped, myself.
I read a study a few years back that found some women still had iron deficiency symptoms even as high as 60 on the ferritin test. Also was pointed out the "normal" scale for iron was devised the way most things were in the past - on healthy college age white males.
What is problematic about the ferritin test is it is treated like a yes/no rather than a continuum. Get 14 on the rest that where 10 is anemia and could be told it's not iron deficiency.
The best advice is likely "if you have the symptoms of iron deficiency, treat it".
It's definitely one of the most prevalent health problems affecting women globally.
It really is horrific just how many women suffer needlessly from it, when a pill and a vitamin C can work wonders.
When people come to us (GPs/Family Physicians) with hair loss for example, the first thing a doctor would do would be to check their bloods, specifically looking for ferritin levels (and other things eg thyroid etc).
If the ferritin level is less than 60 then we would recommend increasing their iron intake.
Thinking about this logically, one could say that the usual lower threshold of normal iron(around 20, differss with age/sex and lab) Is too low if you can increased chances of hair loss at levels below 60, hence I recommend a goal of ferritin > 60.
I recommend that people purchase(in the UK) Ferrous Fumurate (has better bioavailabilty than ferrous sulphate), the more you take the better (upto 3 times a day; you may have GI side effects - abdo discomfort, diarrhoea/constipation/black faeces) and take with 200mg+ of Vitamin C (or fresh orange juice) which triples the absorption of iron, and don't have tea/coffee/dairy one hour either side of taking it (which reduces absorption).
Some other comments brought up that the heme iron in meat is better absorbed, which is true, see figure 1. But the good news is that Impossible burgers have heme iron. They make it in yeast by adding a plasmid with the heme biosynthesis enzymes, pathway in Figure 1 of their patent on the 56th page of the pdf.
Also oysters and mussels can have a decent amount of presumably heme iron, and they seem unlikely to be significantly sentient, and either way, your effects on wild arthropods are more important in your diet choices. I'm vegan except for bivalves.
I didn't keep good track of them, but this post led to me receiving many DMs that it had motivated someone to get tested. I also occasionally indirectly hear about people who got tested, so I think the total impact might be up to 100 people, of which maybe 1/3 had a deficiency (wide confidence intervals on both numbers). I'm very happy with that impact.
I do wish I'd created a better title. The current one is very generic, and breaks LW's "aim to inform not persuade" guideline.
If anyone's tracking impact, my family had five people tested due in large part due to this post, of whom five were low and started supplementing. We're not even vegan.
Maybe this is off topic, but if I'm getting tested for iron deficiency, are there other tests it would make sense to do at the same time (if I'm vegan)? I'm optimizing for minimizing number of doctor's visits/blood draws rather than minimizing cost.
I haven't quantified these, but the other classic vegan deficiencies are Vitamin D and B12. Examine.com has a decent guide to veganism, although I find them less than totally thorough.
You can donate blood which has other health benefits and they will tell you blood ferritin since they need to test that to allow you to donate. If you are iron deficient they will turn you away.
The LessWrong Review runs every year to select the posts that have most stood the test of time. This post is not yet eligible for review, but will be at the end of 2024. The top fifty or so posts are featured prominently on the site throughout the year.
Hopefully, the review is better than karma at judging enduring value. If we have accurate prediction markets on the review results, maybe we can have better incentives on LessWrong today. Will this post make the top fifty?
I recommend to my patients to purchase(in the UK) Ferrous Fumurate (has better bioavailabilty than ferrous sulphate), the more you take the better (upto 3 times a day, you may have GI side effects) and take with 200mg+ of Vitamin C (or fresh orange juice), and don't have tea/coffee/dairy one hour either side of taking it.
(I'm a GP/Family Physician)
I read that Copper deficiency can impact Iron absorption (causing deficiency). Zinc supplementation can cause Copper Deficiency.
Donating blood is a free way to get your hemoglobin levels measured (although, it removes your iron so you shouldn't do it if you are deficient, and should supplement with iron afterwards). I donate about every 3 months for altruistic reasons.
I should also emphasize that it's very possible to overdose on iron (especially if supplementing it) so be careful!
In brief
Recently I became interested in what kind of costs were inflicted by iron deficiency, so I looked up studies until I got tired. This was not an exhaustive search, but the results are so striking that even with wide error bars I found them compelling. So compelling I wrote up a post with an algorithm for treating iron deficiency while minimizing the chance of poisoning yourself. I’ve put the algorithm and a summary of potential gains first to get your attention, but if you’re considering acting on this I strongly encourage you to continue reading to the rest of the post where I provide the evidence for my beliefs.
Tl;dr: If you are vegan or menstruate regularly, there’s a 10-50% chance you are iron deficient. Excess iron is dangerous so you shouldn’t supplement blindly, but deficiency is easy and cheap to diagnose with a common blood test. If you are deficient, iron supplementation is also easy and cheap and could give you a half standard deviation boost on multiple cognitive metrics (plus any exercise will be more effective). Due to the many uses of iron in the body, I expect moderate improvements in many areas, although how much and where will vary by person.
Note that I’m not a doctor and even if I was there isn’t good data on this, so it’s all pretty fuzzy. The following is an algorithm for treating iron deficiency that I’ve kludged together from various doctors. I strongly believe it is a lot better than nothing on average, but individuals vary a lot and you might be unlucky.
[Note: I provided links to supplements because I found people follow through more when I do, and because it’s easy to buy worthless supplements. There are other good supplements out there and if you have a reason to prefer one, take that instead. Links are affiliate.]
Research summary
Iron’s most famous use in the body is in hemoglobin, which your blood uses to transport oxygen. Oxygen is extremely important [citation needed], so it makes sense that low hemoglobin (aka anemia) gets a lot of attention, and everyone agrees anemia is very bad. But what the studies I read found was that even among people who started with adequate hemoglobin, a low ferritin score still predicted they would benefit from supplementation. And it’s not because of a bad definition of “adequate”; people saw benefits even when their hemoglobin didn’t change. So what else does iron do?
Iron is one of a small number of elements that can safely accept electrons in reduction-oxidation reactions. Free electrons are quite damaging, so iron’s ability to safely contain them is important. Some specific usages:
I’d say “that’s a lot” but honestly it’s not, everything in the body is like this, it was not built to be understood.
Standard tests for anemia only look at hemoglobin. Ferritin tests are considered to be a much better measurement of cellular iron levels. There’s suspicion, although not proof, that your body prioritizes hemoglobin production above other uses of iron, so it will undersupply these other uses in order to maintain hemoglobin levels. This suggests that if you have normal hemoglobin but low ferritin, additional iron will find many uses. Unfortunately, those uses and their effects are so varied I can’t really predict what any particular person will experience.
There are any number of studies showing correlations between low ferritin and low functioning, but I don’t find those very useful. The people in those studies might have any number of deficiencies for multiple reasons, or low ferritin levels could just be a proxy for poverty. In my research I stuck to actual experiments, with controls, that gave iron to subjects and checked for an improvement in function, not just test scores. Unfortunately, there were not that many of them.
The only study I liked on the cognitive effects found an absolutely enormous effect. Successful iron supplementation led to improvements averaging >0.5 standard deviations in attention, learning, and memory. I have qualms about this study and expect the results are cherrypicked, but it’s also not necessarily the full size of the effect, because they stopped after a set amount of time rather than waiting for effects to plateau.
There were multiple studies on iron supplementation and exercise. In a nutshell: everyone’s endurance improves when they exercise. Giving people with iron deficiency but not anemia (IDNA) iron supplements increases that effect. In the strongest study, people treated for iron deficiency for 6 weeks improved their 15km time by 10%, compared to 5% in the control group. Another study (which didn’t involve exercise training) showed no improvement in time to complete a given distance, but did find the treatment group used about 5% less energy while doing so.
Iron deficiency rates vary a lot by population, but with the patterns you’d expect. Vegans are more deficient than vegetarians, who are more deficient than omnivores. People who regularly menstruate (or give blood) are more likely to be deficient. I found the baseline rate of omnivorous men in rich countries to be somewhere between 0-11%. For a female omnivore it’s 9-22% (these numbers include people already taking supplements; it’s presumably higher if you don’t). Young female vegans who were not already supplementing were at least 50% deficient, plausibly more. Data for non-supplementing male vegans was not available, but let’s ballpark it at 5-25%, based on the ratio between men and women in the general public.
People in poor countries are much more likely to be iron deficient and anemic, due to poor diet and more physical exertion.
Caveats
I am not a doctor, my most relevant credential is a BA in a different part of biology, the fact that I couldn’t find a decent resource and had to make it myself is a sign of civilizational inadequacy.
Normally not being a doctor inhibits me from giving medical advice, but I am going to go ahead and say that iron poisoning is extremely bad and not that hard to induce with pills, don’t do that. Iron poisoning is why you need to be careful your kid only gets one multivitamin a day, and why men can’t use women’s multivitamins (which should actually be “menstruator’s multivitamins”, since the relevant issue is monthly blood loss).
The papers are very finicky and boring and this was really important, so I’ve tried to frontload my conclusion. This is a delicate balancing act of readability and accuracy. I did my best but some trade-offs are unavoidable.
This lit review was done with a focus on people with low iron intake, especially vegans. None of the studies I looked at filtered on dietary intake versus absorption issues. This means they probably underestimate the impact of supplementing for healthy people.
Do not take the dosages in the studies literally, especially if you don’t menstruate. The right dosage depends on the form and your personal needs. I suggest operating based on RDA percentages rather than raw chemical weights.
Details
Definitions
There are a lot of ways to measure iron and iron-related levels in the body. The two most important are hemoglobin (the protein red blood cells use to carry oxygen) and ferritin (the protein your cells use to store oxygen, but also present in blood). There are some other numbers I’m going to ignore.
Hemoglobin and ferritin are both testable via blood sample, and the tests have something called “reference ranges”, which are supposed to be the healthy range of values. Whether the ranges actually capture that is a matter of great controversy, with various people alleging the minimum is what you need to avoid hardcore deficiency diseases, but won’t get you optimum functioning, to people claiming low scores are fine and anyone who says otherwise is a psyop from Big Vitamin. And then there’s individual variation.
Hemoglobin’s reference range is 120g/L-170g/L. Ferritin’s reference range starts between 10 and 20 ug/L, and ends at 150-200ug/L, depending on who you ask. It’s possible to have low hemoglobin (aka anemia) without an iron deficiency or vice versa. Low hemoglobin with adequate iron typically means you’re having trouble manufacturing hemoglobin and is beyond the scope of this post. Low iron with adequate hemoglobin is more controversial. Top explanations include “the tests aren’t that good”, “you’re deficient but your body is prioritizing hemoglobin production”, “you’re about to develop anemia” and “low iron is fine, actually”.
Impact Data
When looking at studies I used the following selection criteria:
This didn’t leave a lot of studies, and I had to accept some other flaws.
Mental
Murray-Kolb and Beard (2007)
This study was by far the best study of cognitive function, maybe the only one that tested an intervention rather than merely looking at correlations. I don’t love it. The data presentation is obviously leaving a lot of information out, I assume to dramatize results. But those results are very dramatic.
This study allowed for mild anemia (hb < 120 but >105), but separated anemic and non-anemic subjects. The paper, uh, doesn’t mention its threshold for iron deficiency; another paper from the same authors set it at serum ferritin <=12ug/L, which is in line with the aggregated averages.
The study included a double control group that started with sufficient iron and hemoglobin. Each group (no deficiency (n=42), iron deficiency without anemia (n=73), and iron deficiency with anemia (n=34)) was split into treatment and placebo groups.
Iron supplementation increased ferritin levels in everyone. People with iron deficiency without anemia (IDNA) increased serum ferritin (sFt in the table) 2.5x more than their placebo group; people with iron deficiency and anemia (IDA) improved ferritin levels almost 4x more than their placebos. Neither group got anywhere close to the ferritin levels of the no-deficiencies group. The treatment group was given 160 mg of ferrous iron daily.
In baseline cognitive testing, IDNA women scored about the same or slightly worse as healthy women, and IDA women scored much worse than both. This is probably an underestimate of the effect, because the study was heavily recruited from students at a single university, who can be expected to be selected for the same range of competence.
The study separately evaluated treatment-group women who had increased ferritin levels from those who didn’t. The former group had large improvements in their cognitive test results, the latter very modest ones. I think separating out non-responders is fair: if there’s a problem interfering with iron absorption that doesn’t tell you anything about the effect of increasing ferritin levels, and I am studying this mostly for the benefit of people with insufficient dietary intake.
Among ferritin responders, attention, memory, and learning increased from .5 to .75 standard deviations (although somehow that .75 is at p<0.07). That effect size is the equivalent of 7.5-12.5 IQ points or 1.1-1.6 inches in height. Of course the test could be bullshit, but it’s not out of line with anecdotes I hear. Additionally, the treatment groups did not reach the ferritin levels of the healthy group, indicating potentially more gains to be had.
Hemoglobin responders also saw more improvement than non-responders, but the effect size was smaller than with ferritin, indicating an effect of iron beyond increasing hemoglobin.
(Note that the axis has changed from performance to time required, making negatives good. Yes, I am suspicious that they presented total score for one metric and time to completion for another).
Physical
Zhu and Haas (1998)
20 women with normal hemoglobin (Hb >120 g/l) but low ferritin (serum ferritin <= 16 ug/l) were given 135 mg ferrous iron supplements for eight weeks and instructed to take with citrus juice. 17 women were given placebos as a control (random assignment, double-blinded). They were given both blood and athletic tests before and after treatment.
Treatment group hemoglobin and iron binding capacity were unchanged. Serum ferritin was up 250% for the treatment group (compared to 30% for the control). Their athletic test results did not improve any faster than the controls, however they needed less energy (2.0kj/min) and oxygen (5%) to get those same results.
Hinton et al (2000)
22 women with normal hemoglobin (Hb >12 g/dl) but low ferritin (serum ferritin <= 16 ug/l) were given 100mg ferrous iron supplements for six weeks. 20 women were given placebos as a control (random assignment, double-blinded). They were given both blood and athletic tests before and after treatment.
Iron supplementation did not change hemoglobin or iron binding capacity levels, but did increase serum ferritin by about 50%, and transferrin saturation by 70%. Note that their ending ferritin levels (19.4) were still barely above the bottom of the reference range, indicating there was probably much more room for growth.
The control group went marginally up on some measurements and marginally down on others, I’ve treated their changes as noise.
Both treatment and placebo groups were given 4 weeks of exercise treatment; the treatment group showed about double the athletic improvement. Endurance saw a bigger improvement than initial performance.
Brownlie et all (2004)
~20 women, with serum ferritin concentration < 16 ug/L and a hemoglobin concentration > 120 g/L were given 100mg ferrous iron/day for 6 weeks. Of that, 4 weeks also included exercise training.
Once again we see an improvement in ferritin but not hemoglobin or binding capacity.
The treatment group experienced ~30% more improvement in their trial times than the control, or 800% if they started with elevated ferritin. I’m suspicious of this posthoc subgroup analysis, but on the other hand, the bar in this graph is very big.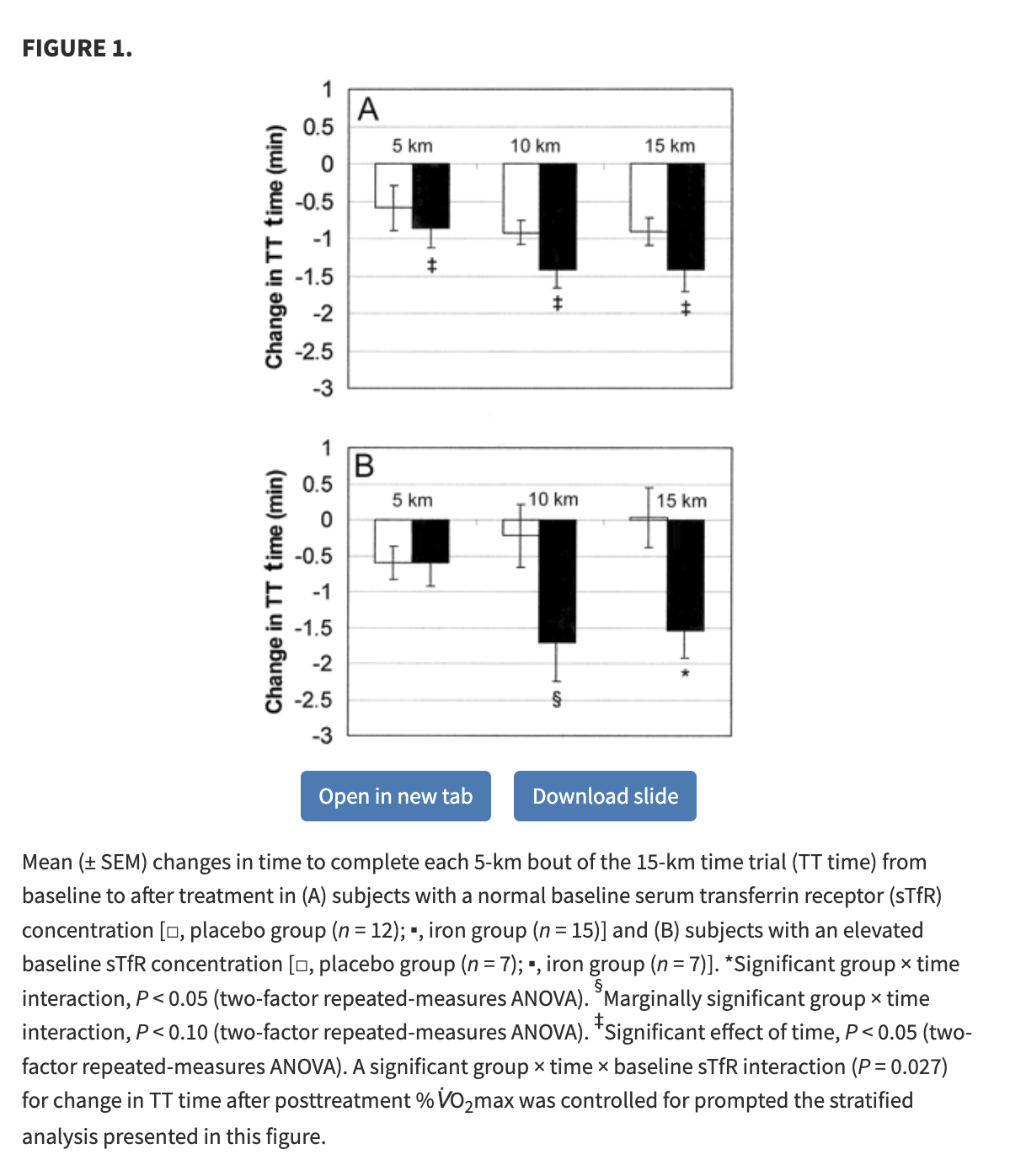
Hinton and Sinclair (2006)
The good news: this study has men! I did not think I was going to find any of those!
The bad news: this study has 20 people, total.
No meaningful change in hemoglobin or binding capacity, near doubling of serum ferritin in the treatment group, 15% drop in ferritin in the control group.
Results are basically identical for the control and placebo groups.
Prevalence Data
Estimates for the prevalence of iron deficiency vary a lot by study and population.
In the first paper I found, the estimate was 9-22% among menstruating women in the general public, and 1-2% among adult men (non-menstruating women were not included but I expect “do you lose 2-4 tablespoons of blood every month?” and “do you occasionally host demanding parasites?” to be more important than hormones or gender identification). Note that this number includes both anemic and non-anemic iron deficiency.
Vegans are at much more risk. One German study of vegan women found a median serum ferritin level of 14 ug/L, a level that is above their reference range and LabCorp’s but below the cut-off in several of the studies cited above. They found 40% of young women fell below their threshold for deficiency (12ng/ml) and 11% of older women (presumably mostly post-menopausal) did so. Women taking iron supplements were excluded from this study.
A second German study (why are they all from Germany?) that allowed supplements and had an even gender split found rates of iron deficiency slightly lower in vegans than omnivores, but both had higher means than anyone in any of the impact studies I found. Nonetheless, 10% of vegans were iron deficient.
My own study (data forthcoming) had 3-4 male vegans and a deficiency rate of 25%-75%, depending on how you count.
Thank you to the Survival and Flourishing Fund for funding this research and Lightcone Infrastructure for providing a home for it.