What is the typical course of COVID-19? What are the variants?
28Elizabeth
25Elizabeth
11Lukas_Gloor
2Elizabeth
2Davidmanheim
2Davidmanheim
23Elizabeth
1Lukas_Gloor
13Elizabeth
4Eli Tyre
2Elizabeth
4Elizabeth
4Elizabeth
3Elizabeth
-3Davidmanheim
10Raemon
4Elizabeth
4Elizabeth
0Davidmanheim
4Elizabeth
4ozziegooen
4Dagon
2Elizabeth
2Dagon
2Pattern
2DanielFilan
2habryka
New Answer
New Comment
8 Answers sorted by
280
Early Appearance of Symptoms
Tl;dr COVID-19 might start with a cough, or a fever, or both, or occasionally maybe neither. It might start suddenly or slowly. It might remit and then come back worse.
This was hard to figure out. Most academic/medical papers start with the person’s first contact with the medical system, which is too late, so I looked at social media and news reports. These are obviously going to be biased towards people with symptoms severe enough to be interesting, but not so severe as to die. I also restricted myself to test-confirmed cases, which because I was also looking at mostly American sources biases things towards severe cases. And I’m counting on people to represent themselves honestly. So there’s a lot going against this sample.
In total I found 11 cases, plus two notes from doctors doing front line work. You can see my and Eli Tyre’s notes on every case here and the symptom tracking spreadsheet here. Both are messy and no work has been spent making them comprehensible to others.
From this very small and biased sample:
- 36% of people started with a cough on their first day (55% if you count two people who had very mild symptoms on day 1 and developed a cough on day 2)
- 64% started with a fever.
- 18% of people started with both on the same day.
- 18% started with neither symptom (but developed a cough on day 2)
- 78% eventually developed a cough
- 91% eventually developed a fever. The only person who didn’t eventually develop a fever I think might be a false positive, because his symptoms were very weird.
- 27% had digestive symptoms (mostly nausea)
- ⅓ of recovered people had been hospitalized.
On the other hand, this pre-print found that only 44% of patients had a fever on admission to the hospital, and 88% ever had one. The fevers can be intermittent. Both that paper and the doctor I just linked to report very high occurrence (85%+) of lymphocytopenia (low white blood cell count), but that is not very useful to diagnosing yourself, and it’s not clear when it starts.
Known scientific source Business Insider says that most cases start with fever. They do not mention their source.
Commonly Repeated Things I Don’t Believe
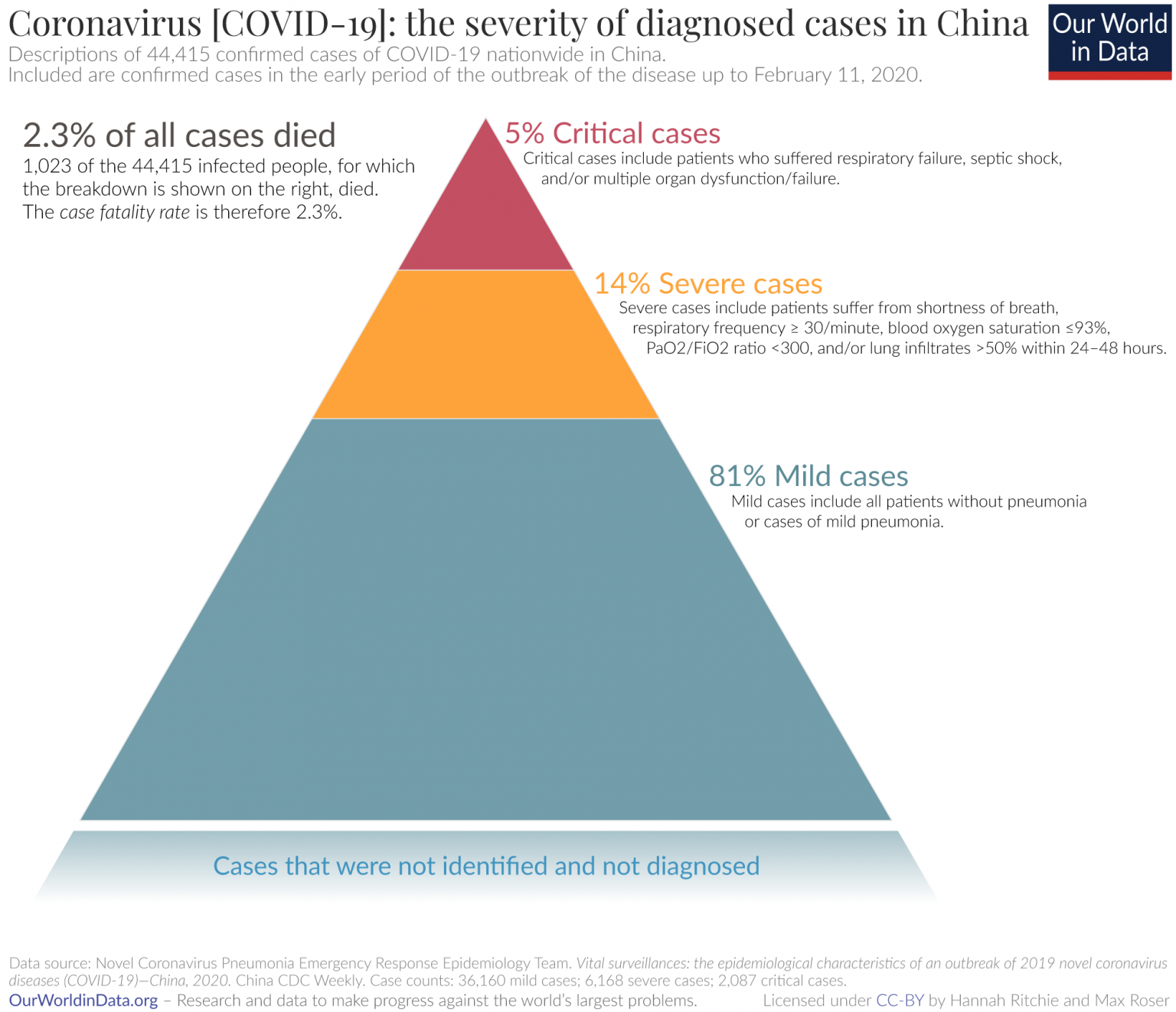
You may have heard that 80% of cases are mild. Keep in mind that that paper defined mild to include mild pneumonia, which I would classify as at least moderately severe.
Similarly, the paper reporting 50% of patients appeared at the hospital with digestive symptoms counted “loss of appetite” as a digestive symptom. Only 19% presented with a more definitely gastroenteric complaint like nausea or vomiting.
*
250What percentage of infections never develop symptoms?
Epistemic Status: Pretty confident in my uncertainty, expect more data to become available that eventually resolves the question
Tl;dr: Anything from zero to half of coronavirus infections are asymptomatic, but we currently can’t narrow it down much more than that.
One way to estimate the number of asymptomatic cases is to PCR test a bunch of people and see what percentage test negative. There’s three obvious problems with that:
- Unrepresentative samples- if you did this in the US the asymptomatic rate would be severely depressed because symptomatics are prioritized in testing.
- Some of those people might go on to develop symptoms later.
- The test could be wrong.
The most representative sample I know of is the Diamond Princess cruise liner, because everyone on board was tested, giving us some kind of reasonable denominator. It’s still not a random sample of the population, because cruise takers skew old-but-healthy-for-their-age, but it’s a start. Of that population, 3,063 tests returned 634 positive results, of which 306 were asymptomatic. But this only solves problem 1, a bit.
This pre-print uses statistical modeling to try to sort those into presymptomatic and true-asymptomatic cases, but has a weird math error I’m trying to get clarity on. I e-mailed the English-speaking author on 3/24 and will update if I hear back, but until then, here’s the problem: the model uses an incubation period of 6.4 to predict that 18% of C19 infections are true-asymptomatic (as opposed to merely pre-symptomatic). But when they let that vary from 5.5 to 9.5 days, they get a range of 20% to to 40%. That only works if percent-asymptomatic is a non-monotonic function of incubation period, and that would be extremely weird..
Even if that model is correct there’s still the problem of unreliable tests. This paper estimates that “almost half or more” of asymptomatic positives among people, tested in China, because they were in close contact with a known case, were false positives and the person never had the virus. Unfortunately the English abstract doesn’t specify how they came to this number, and the original article is in Chinese, so I can’t even attempt to translate this to other populations.
[EDIT 3/28: This paper has been retracted]
This news article based on “classified Chinese government data” says that ⅓ of people who tested positive asymptomatic, but doesn’t specify whether they were monitored to see if they stayed asymptomatic.
My best hope for better data on this is South Korea, thanks to its aggressive testing and monitoring strategy. Unfortunately I haven’t found any of their results, despite spending 30 minutes looking.
Excellent analysis! I've used the 18% point estimate from that Diamond Princess study without noticing that the math could be off.
One point to add: I've seen people say that asymptomatic presentations of SARS-CoV-2 infection might more common in young people, especially in the age range from 20-40. That age range was underrepresented on the cruise ship. For that reason, perhaps it's possible for up to 65% of cases to be asymptomatic?
That said, I very much agree with you that the entire thing about asymptomatic presentations could be a myth based on false positives and confusing "asymptomatic" with "pre-symptomatic." This study is the type of thing that would give us confidence in the existence of asymptomatic carriers – if only it had more examples than just one person.
2
I can't rule out it being 65%, or even higher. I would judge it as pretty unlikely, since I expect many of the asymptomatics on the Diamond Princess to in fact be presymptomatic.
2
They kept them there for long enough that this seems unlikely.
*
230Diamond Princess data. This dataset is particularly useful because everyone on board the ship was tested, meaning asymptomatic infections could be caught. (h/t @habryka for link)

This shows that deaths peak 4 days after hospitalization and then have a long tail. Time to hospitalization is not specified.
Shows the # of asymptomatic cases by age group. I couldn't determine how long after exposure these people were tested, so this should be treated as an upper bound for percent-asymptomatic, not the average. One interesting thing is that people in their 20s and 30s had a much higher rate of symptoms (80%+) than older or younger people (< 60%).
One interesting thing is that people in their 20s and 30s had a much higher rate of symptoms (80%+) than older or younger people (< 60%).
That's indeed interesting. This article seems to say that it's different in young people who tested positive in South Korea.
One point of criticism about the link included under "Diamond Princess data:"
The abstract reads as follows:
Comparing deaths onboard with expected deaths based on naive CFR estimates using China data, we estimate IFR and CFR in China to be 0.5% (95% CI: 0.2–1.2%) and 1....
130
Day by day course of coronavirus, starting from day 1 of symptoms
Day 1: Patients run a fever. They may also experience fatigue, muscle pain, and a dry cough. A small minority may have had diarrhea or nausea one to two days before.
Day 5: Patients may have difficulty breathing — especially if they are older or have a preexisting health condition.
Day 7: This is how long it takes, on average, before patients are admitted to a hospital, according to the Wuhan University study.
Day 8: At this point, patients with severe cases (15%, according to the Chinese CDC) develop acute respiratory distress syndrome, an illness that occurs when fluid builds up the lungs. ARDS is often fatal.
Day 10: If patients have worsening symptoms, this is the time in the disease's progression when they're most likely to be admitted to the ICU. These patients probably have more abdominal pain and appetite loss than patients with milder cases. Only a small fraction die: The current fatality rate hovers at about 2%.
Day 17: On average, people who recover from the virus are discharged from the hospital after 2 1/2 weeks.
It would be great if we knew at what point in this process people are typically "confirmed as having COVID-19", for modeling the lag between time of infection and time of diagnosis.
Do people only get "confirmed" after they've been admitted to a hospital?
2
I think it varies by country. My impression is that for the US you have to be very ill, but Korea is doing drive by testing.
40
From Our World In Data based on this paper. It's not clear that they studied people until recovery, so some of those mild cases could have gotten more serious later.
40
First-person account from a woman who believes she and many other people were infected at a party. She was confirmed positive via the Seattle Flu Study, the other victims were not.
40% of folks were all sick within 3 days of attending the party all with the same/similar symptoms including fever.
Most of my friends who got it were in their late 40s to early 50s. I’m in my mid 30s. For us it was headache, fever (for first 3 days consistently and then on and off after 3 days), severe body aches and joint pain, and severe fatigue. I had a fever that spiked the first night to 103 degrees and eventually came down to 100 and then low grade 99.5. Some folks had diarrhea. I felt nauseous one day. Once the fever is gone some were left with nasal congestion, sore throat. Only a very few of us had a mild itchy cough. Very few had chest tightness or other respiratory symptoms. Total duration of illness was 10-16 days.
30
A pre-print out of Germany on a study of 9 patients shows:
- Individuals were shedding high levels viral RNA once they were symptomatic (pre-symptomatic case not tested)
- Throat, lung, and stool samples all contained viral RNA, but only throat and lung samples could be cultured to produce new virus. Blood and urine did not yield viral RNA.
- Shedding of viral RNA from sputum outlasted the end of symptoms.
- Seroconversion occurred after 6-12 days of symptoms, but was not followed by a rapid decline in viral loads.
-30
The CDC has a lot of useful information about much of this: https://www.cdc.gov/coronavirus/2019-ncov/about/index.html
For example, on the clinical course of the disease, it has this: https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-guidance-management-patients.html#clinical-course - "Clinical presentation among reported cases of COVID-19 varies in severity from asymptomatic infection to mild illness to severe or fatal illness. Some reports suggest the potential for clinical deterioration during the second week of illness.[2,5] In one report, among patients with confirmed COVID-19 and pneumonia, just over half of patients developed dyspnea a median of 8 days after illness onset (range: 5–13 days). [2] In another report, the mean time from illness onset to hospital admission with pneumonia was 9 days.[1] Acute respiratory distress syndrome (ARDS) developed in 17–29% of hospitalized patients, and secondary infection developed in 10%. [2,4] In one report, the median time from symptom onset to ARDS was 8 days.[3]"
For information about when someone is infectious, https://www.cdc.gov/coronavirus/2019-ncov/hcp/faq.html, it says, "The onset and duration of viral shedding and period of infectiousness for COVID-19 are not yet known. It is possible that SARS-CoV-2 RNA may be detectable in the upper or lower respiratory tract for weeks after illness onset, similar to infection with MERS-CoV and SARS-CoV. However, detection of viral RNA does not necessarily mean that infectious virus is present. Asymptomatic infection with SARS-CoV-2 has been reported, but it is not yet known what role asymptomatic infection plays in transmission. Similarly, the role of pre-symptomatic transmission (infection detection during the incubation period prior to illness onset) is unknown. Existing literature regarding SARS-CoV-2 and other coronaviruses (e.g. MERS-CoV, SARS-CoV) suggest that the incubation period may range from 2–14 days."
For information about how to tell when someone is no longer infectious, see: https://www.cdc.gov/coronavirus/2019-ncov/hcp/disposition-hospitalized-patients.html
They also have a frequently updated list of papers that have the sources for their information: https://www.cdc.gov/coronavirus/2019-ncov/publications.html
Thanks!
I found this slightly hard to parse (for the reasons I find academic papers generally hard to parse), and have re-written it here to be slightly easier for me:
For example, on the clinical course of the disease, it has this: https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-guidance-management-patients.html#clinical-course
Clinical presentation among reported cases of COVID-19 varies in severity from asymptomatic infection to mild illness to severe or fatal illness.
Some reports suggest the potential for clinical deterioration during the second week of illness. In one report, among patients with confirmed COVID-19 and pneumonia, just over half of patients developed dyspnea a median of 8 days after illness onset (range: 5–13 days).
In another report, the mean time from illness onset to hospital admission with pneumonia was 9 days. Acute respiratory distress syndrome (ARDS) developed in 17–29% of hospitalized patients, and secondary infection developed in 10%. In one report, the median time from symptom onset to ARDS was 8 days.
For information about when someone is infectious, https://www.cdc.gov/coronavirus/2019-ncov/hcp/faq.html, it says
The onset and durat
I don't see where the second- and third-to-last links contain information on contagiousness. To make sure I'm not missing something:
- the section under "when someone is infectious" says "The onset and duration of viral shedding and period of infectiousness for COVID-19 are not yet known"
- Interim Guidance for Discontinuation of Transmission-Based Precautions and Disposition of Hospitalized Patients with COVID-19 contains considerations, but not instructions, for when to discontinue isolation, and nothing directly on when people
4
For anyone just tuning in, David Manheim and I have a pre-existing dispute over the usefulness of CDC-given information. I'm going to leave this up because others might find it useful, and I'm not going to respond directly because there's no reason to expect it to go differently than the last 5 times we discussed the CDC, but I do think he's wrong.
0
If you are asking about the R_0, there is a lot of information that you're mentioned elsewhere. If you're asking about infectiousness time periods, CDC has information that you just cited. You're looking for numerical epidemiological estimates - and the papers on the epidemiology that CDC cites are very clear that they don't have that good data. Do you want a proxy for modeling purposes? Feel free to use any of the guesses provided in the literature so far, but note that most places where data might have existed that could inform this are locked down, so there would be fairly little data to indicate if now-formerly infected people are still transmitting the disease.
So you're asking for information that experts say is currently unknown. That means any supposed "answers" to how long the infectiousness period lasts that have been published so far are going to be misleading. And knowing that a clear answer doesn't exist is valuable information - it means you can stop sources like businessinsider stating that on average after 17 days people who recover are released from the hospital - which may be a correct average, but as the CDC's explanation about the need for testing viral load in individual cases before release from in-home isolation makes clear, tells you nothing about how long they remain infectious.
Rendering 8/19 comments, sorted by (show more) Click to highlight new comments since:
VALUE OF INFORMATION
Say I have the option to purchase a lottery ticket with a 1/10m chance of winning, a $1m guaranteed jackpot, and a $1 ticket price. The EV of a ticket is $1m/10m - $1 = -$0.9, a bad deal. What is the value of information that narrows the odds?
If it narrowed the odds all the way to 1/1, the value would be $999,999, obviously a very good deal. I should be willing to pay up to almost $999,999 for it.
But if the odds are doubled? The EV of a purchase is now $1/5-$1 = -$0.80. In one sense I’ve gained $0.1. But since buying a lottery ticket is still EV < 0, I won’t purchase one, and so the information nets me no money. The information is worth $0 to me, as long as I have the option not to buy a ticket.
But… maybe there are multiple interventions that double my odds? Under the above rule, the first three are worth nothing and the fourth is worth $2^4/10 - $1 = $0.6. It seems wrong that 4 identical interventions would have such different values. I could just divide .6 by 4, but what if I’m not certain how many doublings will be available?
Interesting point. I think this is more a question of counterfactual and Shapely values than VOI, as the concern is really a broader one. Similar how to if 4 interventions are all needed to save a life, you can't just consider the counterfactual impact of the last one.
Most VOI analyses are highly simplified to get around issues like this.
If the interventions have aggregate impact distinct from individual impact, they're by definition not identical. There are lots of things that are valuable only in conjunction with other things, or have threshold values for quantities - it doesn't seem problematic to say "any of these interventions is valueless, but all 4 together are worth $0.6 per $1 I have to invest".
If the interventions have aggregate impact distinct from individual impact, they're by definition not identical
Why not? I don't see how that follows.
It's not an important point - the value of aggregates being different from a simple sum of the components is mostly what I meant to say.
The interventions may be identical for some kinds of measurement, that is, they "feel" the same to the user. But they're not actually identical if they're applied to different states of the world and have different results from each other.
"Rationality" is pretending you can model (despite) uncertainty, and making a model.
'If you start with a prior' sounds great - unless you don't have a prior.
I'm going to take the easy way out and say that if you did have a prior, then maybe upon finding there is such an 'intervention', since that's probably more likely in worlds where there are more interventions*...and I just realized the value of information problem is both object level and meta.
*Then you update, in theory.